
Central Precocious Puberty: Puberty Before Its Time
Actor Portrayals
CPP is when puberty
starts too soon
While puberty is a normal part of growing up, some children may go through puberty sooner than expected. This condition is called central precocious puberty, or CPP

before
age 8
in girls

before
age 9
in boys
CPP is rare, affecting only 1 in 5000 to 1 in 10,000 children in the United States, and is 10x to 20x more common in girls than boys
How does puberty start?
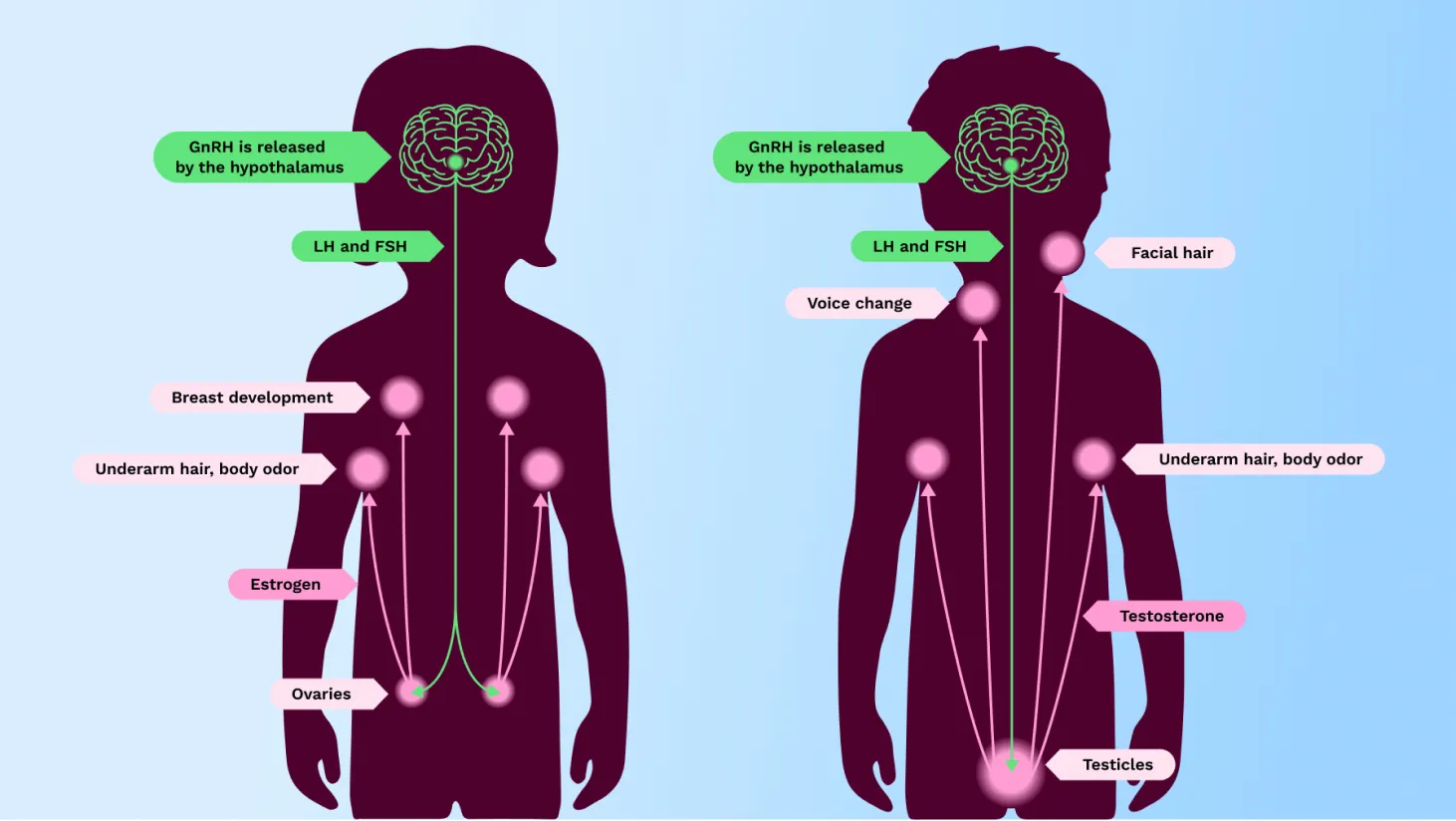




Common signs of puberty in girls
- Breast development
- Menstrual period
- Pubic or underarm hair
- Oily skin/acne
- Adult body odor
- Sudden growth spurt
Common signs of puberty in boys
- Testicle and penis enlargement
- Erections
- Voice change
- Facial hair
- Muscle growth
- Pubic or underarm hair
- Oily skin/acne
- Adult body odor
- Sudden growth spurt
How does CPP affect children?
Growth and height
CPP can affect your child’s height in 2 ways:
- A child with CPP may go through an early growth spurt and be taller than other children the same age
- Children with CPP that go untreated may end up shorter than they should be as adults. This is because their bones start maturing too soon, and their growth plates fuse, or close, too early. As a result, their bones stop growing sooner than they should
Social and emotional impacts
Girls and boys who begin puberty before their peers may be extremely self-conscious about the changes occurring in their bodies. This may affect their self-esteem and may increase their risk of developing depression, eating disorders, or substance abuse, perhaps as a result of standing out before they’re ready for the extra attention.
There are no data demonstrating outcomes of Triptodur on stature, social, or emotional health.

How is CPP diagnosed?
If your child’s healthcare provider is concerned that your child may have CPP, your child will most likely see a pediatric endocrinologist for a diagnosis. A pediatric endocrinologist is a children’s doctor specializing in diagnosing, treating, and managing disorders involving hormones, including CPP.
Some of the tests and exams used to diagnose CPP may include
Blood tests to measure hormone levels, including a test called a GnRH stimulation test. In children with CPP, the GnRH stimulation test will cause other hormone levels in the body to rise. In children without CPP, these hormone levels will stay the same.


An X-ray of the left hand and wrist to measure how fast your child’s bones are growing (referred to as your child’s bone age).
A physical exam to observe whether your daughter is developing breasts or whether your son’s testicles are starting to get larger, as well as other signs of puberty, such as body odor, acne, and whether pubic hair is starting to grow.
How is CPP treated?





How to talk to your child about CPP
Children with CPP may have a hard time understanding the changes taking place in their bodies, such as the growth of pubic or underarm hair, the appearance of acne, or the development of body odor. Girls may be upset to see their breasts growing or to get their first period, while boys may be surprised by facial hair or a deepening voice.
It’s not unusual for children with CPP to feel confused or embarrassed by these changes. Because they tend to look older physically, they are often expected to behave more maturely, which can increase the pressure and expectations placed upon them. As a parent, you play a key role in shaping your child’s understanding of CPP and creating a nurturing environment where your child can feel loved and supported.
